Decompression surgery: 5 big myths related to spinal surgery and their truth for better health.
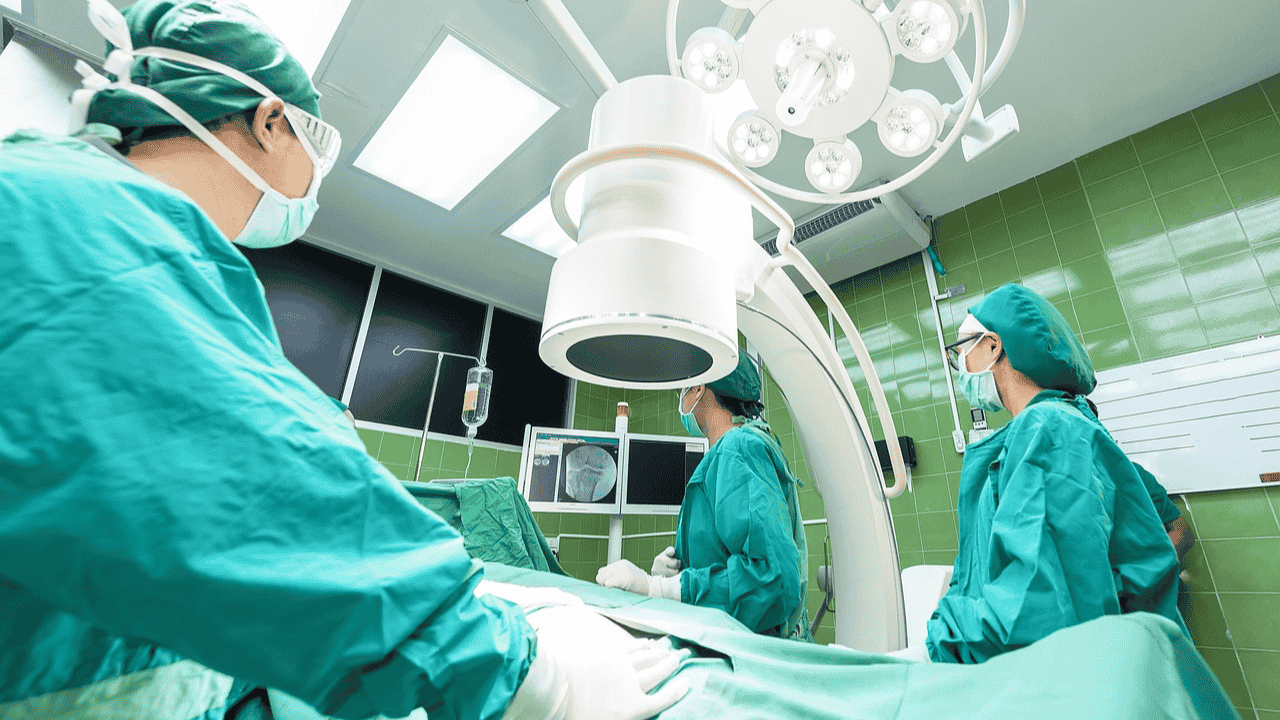
Decompression surgery can be best option if numbness and more pain .When it comes to severe spinal pain or pressure on nerves, doctors may often suggest decompression surgery. This is a procedure in which bone or soft tissue (such as part of a herniated disc) is removed to reduce pressure on the spinal cord or nerves. However, the name of the surgery itself scares many people and many misconceptions are prevalent about it.
Myth 1: Decompression surgery is always dangerous and can cause paralysis.

Truth: This is the biggest and most common myth about decompression surgery. In modern medical science, decompression surgery, especially with minimally invasive techniques, is considered quite safe.
Low risk: Every surgery has some risks, but the risk of paralysis in decompression surgery is very low. Surgeons work very carefully and use advanced techniques.
Purpose: The main purpose of surgery is to relieve symptoms and prevent damage by removing pressure on the nerve or spinal cord, not to cause damage.
Trained surgeons: The procedure is performed by highly trained neurosurgeons or spinal orthopedists.
In fact, if severe nerve compression is not treated, the risk of paralysis or permanent nerve damage is high.
Myth 2: Pain and recovery after decompression surgery is very long and painful.
Fact: This belief is often associated with old surgical techniques. Recovery in modern decompression surgery is much faster and less painful than before.
Minimally invasive techniques (MIS): Many decompression surgeries nowadays are performed using minimally invasive methods, which involve smaller incisions. This causes less damage to the muscles, less bleeding, and faster recovery.
Shorter hospital stay: In many cases, the patient is discharged the same day or within 1-2 days.
Earlier mobility: Patients are often encouraged to move around within a few hours of surgery, which speeds up recovery and reduces the risk of complications.
Pain management: Effective medications are given to control pain after surgery, making patients feel comfortable.
Although recovery time depends on individual factors (such as the type of surgery, the patient’s overall health), it is a misconception that you will have to stay in bed for months.
Myth 3: Once you have spinal surgery, you will never be able to do normal activities again.
Truth: This is completely wrong. The goal of decompression surgery is to get you back to your normal activities.
Improved mobility: Once the pressure on the nerve is relieved by surgery, pain and numbness decrease, allowing you to move better.
Physical Therapy: Physical therapy is often recommended after surgery. It helps strengthen muscles, increase flexibility, and relearn proper physical movements, allowing you to resume your daily routine and favorite activities.
Improved quality of life: Many patients experience a better quality of life after surgery, as they are able to live a more active life, free of pain.
Myth 4: Spine surgery is never successful or the pain always returns.
Truth: Decompression surgery has a high success rate, especially when the right patient is selected and the surgery is done for the right reasons.
High success rate: Decompression surgery for conditions such as leg pain (sciatica) caused by a herniated disc can have a success rate of over 90%.
Recurrence of symptoms: In some cases, symptoms may return over time due to the underlying degenerative process or if patients do not make lifestyle changes. But this does not mean that the first surgery was unsuccessful. It is often a sign of a new problem or progression of an existing condition.
The right choice: For a successful outcome it is important that surgery is performed only when non-surgical treatments fail and the cause of the symptoms can be clearly identified.
Myth 5: Surgery is the only option for a spinal problem.
Fact: Surgery is the last resort for most spinal problems. Doctors always try non-surgical treatments first.
Conservative treatments: This includes things like medications, physiotherapy, heat/cold therapy, exercise, lifestyle changes, and injections.
When is surgery recommended? Surgery is recommended only if conservative treatments are not effective for 6-12 weeks, the pain becomes unbearable, or if there is severe muscle weakness, numbness, or problems with bladder/bowel control due to pressure on the nerve.
Individual decision: The decision to have surgery is an individual decision based on the patient’s condition, severity of symptoms, and lifestyle needs, agreed upon by both the doctor and the patient.










Post Comment